The Covid-19 pandemic has caused immense confusion, fear, and debate since its first outbreak in Wuhan, China in November of 2019. Among the most significant debates surrounding the pandemic has been the origin of the virus. Recently, the U.S. Energy Department released a report stating that COVID-19 “most likely” originated in a lab. This finding suggests that the virus could have been either created or modified in a laboratory, potentially contributing to the pandemic’s emergence. However, it’s crucial to note that the report does not suggest that the outbreak was intentional. In fact, the lab’s intention might have been to reduce the likelihood of a pandemic.
Despite the U.S. Energy Department’s report linking COVID-19 to a lab origin, controversy surrounds the finding as four other government departments maintain that the virus occurred naturally. The Energy Department itself expressed “low confidence” in its report. The FBI also supported the lab leak hypothesis in 2021, but only with “moderate confidence.” Conversely, the National Intelligence Council reported that four anonymous agencies assess with “low confidence” that the virus evolved naturally through transmission from an infected animal. Other government agencies, such as the Central Intelligence Agency, remain undecided between the lab-leak and natural-transmission theories. The ongoing debate underscores the complexity of tracing the origins of the COVID-19 pandemic.
It is worth noting that despite the diverging opinions among government agencies, there is a consensus that COVID-19 was not the result of a Chinese biological-weapons program. The argument is further supported by the fact that three researchers from the Wuhan Institute of Virology became ill in November 2019 and sought hospital care. However, the FBI has been unable to provide any further details regarding the incident due to Justice Department policy aimed at preserving “the integrity of ongoing investigations.” The lack of information adds to the challenges of tracing the virus’s origins, making the situation more complex and uncertain.
In light of the ongoing debate and divergent opinions on the origin of COVID-19, President Biden has called upon the intelligence community to intensify their efforts in investigating the matter. The President has directed that the review draw on work by the U.S.’s national laboratories and other agencies. The complexity of the situation is becoming increasingly apparent, and the answer may not be as straightforward as initially presumed. As the intelligence community continues to scrutinize and analyze the evidence, there is hope that definitive answers will be forthcoming, helping to resolve the global health crisis that has affected millions of lives worldwide.
The Covid-19 pandemic has undoubtedly had a profound and unparalleled impact on the world, highlighting the significance of science, facts, and cooperation in the face of a global crisis. The ongoing debate over the origin of the virus has been a point of contention since its inception, and finding conclusive answers remains crucial in providing solutions to the ongoing pandemic. As we move forward, it is essential to remember the importance of scientific inquiry, objective analysis, and collaboration in finding answers to the most significant challenges of our time.
Keys to a Healthy World: Expanding Access to Healthcare
Access to healthcare is an important factor in keeping individuals healthy and providing them with the medical services they need. Unfortunately, many people around the world do not have access to the healthcare they need due to a variety of factors, such as economic status, geographic location, and limited availability of services. Improving access to healthcare is essential for improving the health of individuals and communities around the world. Several strategies for improving access to healthcare, include expanding healthcare coverage, increasing healthcare availability, improving healthcare affordability, ensuring access to oral health care, and improving access to mental health care.
Expanding Healthcare Coverage
One of the most effective strategies for improving access to healthcare is expanding healthcare coverage. This can be achieved by providing public health insurance, such as Medicare and Medicaid, to more individuals. Additionally, public health insurance programs can be expanded to cover services that are not currently covered, such as dental and vision care. Expanding healthcare coverage can help individuals who otherwise would not have access to medical services receive the care they need.
Increasing Healthcare Availability
Another important strategy for improving access to healthcare is increasing healthcare availability. This can be achieved by increasing the number of healthcare providers, such as doctors and nurses, as well as the number of available healthcare facilities. Additionally, increasing healthcare availability can involve improving the quality of healthcare services and making them more accessible to individuals who may not be able to travel long distances to receive care.
Improving Healthcare Affordability
In addition to expanding healthcare coverage and increasing healthcare availability, improving healthcare affordability is another important strategy for improving access to healthcare. This can be achieved by providing financial assistance for individuals who cannot afford to pay for their healthcare expenses. Additionally, reducing healthcare costs, such as prescription drugs, can make healthcare more affordable for individuals.
Oral Health
Ensuring access to oral health care is an important part of improving access to healthcare. Providing access to dental care can help individuals maintain healthy teeth and gums, as well as detect and treat oral health problems. Additionally, expanding public health insurance coverage to include dental care can help individuals who otherwise would not have access to dental care receive the services they need.
Mental Health
Improving access to mental health care is also essential for improving access to healthcare. This can involve increasing the availability of mental health services and providing financial assistance to individuals who cannot afford to pay for them. Additionally, providing mental health education and awareness campaigns can help reduce the stigma associated with mental illness and encourage individuals to seek the care they need.
Conclusion
Improving access to healthcare is essential for improving the health of individuals and communities around the world. Strategies for improving access to healthcare include expanding healthcare coverage, increasing healthcare availability, improving healthcare affordability, ensuring access to oral health care, and improving access to mental health care. Implementing these strategies can help ensure that individuals have access to the healthcare services they need in order to stay healthy.
Equality in Healthcare: Increasing Access to Care
Access to healthcare is something that many of us take for granted, but for millions of Americans, it’s a luxury they can’t afford. Whether it’s a lack of insurance coverage, prohibitive costs, or geographical barriers, there are a variety of factors that can make it difficult for people to access the medical care they need. In this article, we’ll take a closer look at some of the biggest obstacles to healthcare access in the US, and explore some of the strategies that can be used to overcome them.
The Problems of Coverage and Cost
One of the biggest hurdles to accessing healthcare is a lack of insurance coverage. According to recent estimates, around 27 million Americans are uninsured. For those who do have coverage, rising out-of-pocket costs can also be a major barrier to care. These financial obstacles can make it difficult for people to afford the medical treatments they need, leading many to go without care altogether.
Location, Language, and Socioeconomic Status
Even for those who have insurance coverage and can afford to pay for care, other barriers can still make it difficult to access healthcare. For example, many rural areas in the US are considered “healthcare deserts,” with a shortage of medical providers. This can make it challenging for people in these areas to find the care they need close to home. Additionally, language barriers can make it difficult for non-English speakers to navigate the healthcare system and communicate with providers. Lastly, socioeconomic status plays a big role, where people living in poverty may have less access to healthcare services.
The Consequences of Inadequate Access
When people can’t access the healthcare they need, the consequences can be severe. Without proper medical treatment, illnesses and chronic conditions can go untreated, leading to unnecessary suffering and even death. In addition to physical health consequences, lack of access to healthcare can also have a major impact on mental health, causing stress, anxiety, and depression. Furthermore, it can also have major economic consequences, such as lost income due to missed work and high medical bills.
Strategies for Overcoming Barriers
So, how can we work to overcome the obstacles to healthcare access? One strategy is to increase insurance coverage through Medicaid expansion and the Affordable Care Act. This can help to ensure more people have access to necessary medical services. Additionally, reducing costs through price negotiation and transparency can make healthcare more affordable for individuals. Providing language and cultural competency training for healthcare providers, increasing the number of healthcare providers in underserved areas, and addressing social determinants of health, such as poverty and education, can also help to improve overall health outcomes.
Special Areas of Concern
Two special areas of concern when it comes to expanding access to healthcare are mental health and dental care. Mental health services often have larger coverage gaps compared to other medical services and individuals may have difficulty obtaining necessary care. Dental care is also an area where access is limited, particularly for low-income individuals and those without insurance.
Conclusion
Expanding access to healthcare is essential for ensuring that all individuals have the opportunity to maintain good health. Lack of access to healthcare has significant physical, mental, and economic consequences. By implementing strategies such as increasing insurance coverage, reducing costs, and addressing location and language barriers, we can work towards expanding access to healthcare for all. It is important for policymakers and healthcare providers to prioritize expanding access to healthcare, particularly in special areas such as mental health and dental care. Let’s work together to break down the barriers to healthcare and ensure that everyone has access to the care they need.
Tennis Legend Martina Navratilova Vows to Fight Cancer with All She’s Got
Tennis great Martina Navratilova has recently been diagnosed with both stage one throat and breast cancer, according to her agent. In a statement on the Women’s Tennis Association (WTA) website, Navratilova, 66, described the diagnosis as a “double whammy” but added that it is “serious but still fixable” and that she is hoping for a favorable outcome. Navratilova, who won 59 grand slam titles in her career, has already battled breast cancer in 2010. The latest prognosis is said to be good, and Navratilova will begin treatment this month.
Navratilova’s agent, Mary Greenham, stated that the tennis legend discovered an enlarged lymph node in her neck during the WTA Finals in Fort Worth, Texas, which led to a biopsy and the throat cancer diagnosis. When Navratilova was undergoing throat tests, a suspicious form was found in her breast, which was later diagnosed as cancer. Greenham said that both cancers are in the early stages with good outcomes.
Navratilova enjoyed a long and successful playing career, winning 18 grand slam singles titles, 31 grand slam doubles titles, and 10 grand slam mixed doubles titles. She holds the WTA Tour’s all-time record of 167 titles. After retiring from singles in 1994 at the age of 38, Navratilova continued playing doubles and winning titles into her 40s. She has remained involved in the sport as a coach, broadcaster, and ambassador for the WTA Tour, and has highlighted the importance of preventive checkups to combat specific diseases such as breast cancer.
Navratilova has faced a number of health challenges throughout her life. In September 1982, an acute attack of toxoplasmosis contributed to her defeat in the United States Open tennis tournament. In 1985, Navratilova began wearing glasses due to deteriorating vision. On April 7, 2010, she announced that she was being treated for breast cancer, and in December 2010, she was hospitalized after developing high altitude pulmonary edema while attempting to climb Mount Kilimanjaro in Tanzania.
Despite these challenges, Navratilova has remained a formidable and determined athlete. In her statement on the WTA website, she said that she will “fight with all [she’s] got” in the face of her recent cancer diagnosis. Navratilova was originally scheduled to cover the upcoming Australian Open from the Tennis Channel studio but will now join occasionally via Zoom, according to Greenham.
Pancreatic cancer is a type of cancer that begins in the pancreas, a gland located behind the stomach that helps with digestion and blood sugar control. It is a serious and often deadly disease, with a high mortality rate. In fact, pancreatic cancer is the third leading cause of cancer-related deaths in the United States.

There are several risk factors for pancreatic cancer. Some of these include age (the risk increases with age), being male, smoking, having diabetes, having a family history of pancreatic cancer, having chronic pancreatitis (inflammation of the pancreas), and being obese.
Symptoms of pancreatic cancer can include pain in the upper abdomen or back, jaundice (yellowing of the skin and whites of the eyes), weight loss, loss of appetite, nausea and vomiting, and fatigue. These symptoms can be caused by other conditions as well, so it is important to see a doctor if you are experiencing any of them.
To diagnose pancreatic cancer, a doctor will perform a physical examination and may order blood tests. Imaging tests such as a CT scan, MRI, or ultrasound can also be helpful in diagnosing the disease. Endoscopic ultrasound (EUS) is a specialized test that involves inserting a thin, flexible tube with an ultrasound probe on the end through the mouth and into the stomach. This test can provide detailed images of the pancreas. A biopsy, in which a small sample of tissue is removed and examined under a microscope, can also be used to diagnose pancreatic cancer.
Once pancreatic cancer has been diagnosed, the next step is to determine the stage of the cancer. The stage of a cancer refers to how far it has spread. There are five stages of pancreatic cancer: stage 0, stage I, stage II, stage III, and stage IV. The stage of the cancer will help determine treatment options.
Treatment options for pancreatic cancer can include surgery, chemotherapy, radiation therapy, and clinical trials. Surgery to remove the cancerous tissue is often the first line of treatment, and may involve a procedure called a pancreatectomy or a more extensive surgery called the Whipple procedure. Chemotherapy uses drugs to kill cancer cells, while radiation therapy uses high-energy beams to kill cancer cells. Clinical trials are research studies that test new treatments in people to see if they are safe and effective.
The prognosis (outlook) for pancreatic cancer depends on a number of factors, including the stage of the cancer, the overall health of the patient, and the response to treatment. Survival rates for pancreatic cancer vary depending on the stage of the cancer. For example, the five-year survival rate for stage I pancreatic cancer is about 20%, while the five-year survival rate for stage IV pancreatic cancer is less than 5%.
Living with pancreatic cancer can be difficult, both for the patient and for their loved ones. It is important to have emotional support and to find ways to manage pain and other symptoms. Palliative care and hospice options can also be helpful for those with advanced pancreatic cancer.
Pancreatic cancer is a serious and often deadly disease that can be difficult to detect in its early stages. Risk factors include age, gender, smoking, diabetes, and others. Treatment options include surgery, chemotherapy, radiation therapy, and clinical trials, and the prognosis depends on the stage of the cancer and the overall health of the patient. Coping with pancreatic cancer can be challenging, and it is important to have emotional support and to find ways to manage pain and other symptoms. Despite the seriousness of pancreatic cancer, there is hope for the future, as researchers continue to work on new.
You may think that student debt doesn’t affect you, but it has deleterious implications for society that goes far beyond the students who owe money.
Value of Education
Higher education leads to social and economic benefits. Graduates are more likely to hold a job, maintain a stable family, live healthier and add value to society. Educated individuals commit less crime and utilize less public resources, such as needing welfare assistance. The benefits of education are passed on to the community. But they are prevented by barriers to education, including student debt.
Student Debt Hurts Society
Students, afraid of the burden of debt, are less likely to pursue higher education. When it comes to meeting the needs of society, our workforce is one of our greatest assets. The ability to meet the growing demands of society relies on training workers when and where they are needed most. However, debt is a huge obstacle. Research shows that it deters students from pursuing education causing harm in many areas of society including public health. Let’s use mental health as an example where there is a large unmet need for care.

Need for Mental Health Services
If you have ever needed to find a therapist, you probably know how difficult it is to find one, let alone get an appointment with one that accepts your insurance. Have you ever wondered why that is? Why is it so difficult to train more psychologists to meet the growing demand for services. While the answer to such questions are never straight forward, student debt plays a large role.
Even for the most qualified, motivated students willing to train as mental health providers, can’t afford it. At least not with expected cost and the anticipated starting salary. A typical psychology graduate might gradate with $250,000, and expect to pay nearly $1900 a month for the next 20 years. With a projected starting salary of of around $60,0000, this graduate might struggle to pay expenses and stay above the poverty line.

Civil rights
While all students who owe debt are facing disadvantages, in an article published in the Harvard Law review entitled “Student Debt is a Civil Rights Issue,” Dalie Jimenez and Jonathan Glater Jimenez discuss how the burdens of student debt disproportionately “harm Black and Latino students” and “put students of color further behind.” Debt relief might therefore, help remedy some of the systematic disadvantages they describe.
Fixing the problem
Reforming education and student debt through various programs, such as public education reform, financial reform or student loan forgiveness programs have been proposed as a means for addressing student debt. However, like many other things in the USA, the issue seems to be highly politicized, even though it has important ramifications for society as a whole.
Reducing student debt is important can add value to society. To the extent it can incentivize education, it can stimulate the economy, improve health, strengthen families, reduce crime and ensure we meet the growing needs of our society.
Notes:
1. 250K includes undergraduate + graduate education costs.
Breast Cancer
Breast cancer is a type of cancer that develops in the cells of the breast. It is the most common cancer among women and can also occur in men. Early detection and treatment are important for improving the chances of successful treatment and survival.Types of Breast Cancer
There are several types of breast cancer, including:- Ductal carcinoma in situ (DCIS): DCIS is a non-invasive breast cancer that occurs in the cells lining the breast ducts. It has not spread beyond the ducts and is considered the earliest stage of breast cancer.
- Invasive ductal carcinoma (IDC): IDC is the most common type of breast cancer and occurs in the cells lining the breast ducts. It has the potential to spread to other parts of the body and is classified based on the stage of the cancer (see below for more information on stages).
- Invasive lobular carcinoma (ILC): ILC is a type of breast cancer that occurs in the lobules, which are the glands that produce milk. It has the potential to spread to other parts of the body and is also classified based on the stage of the cancer.
- Inflammatory breast cancer (IBC): IBC is a rare and aggressive type of breast cancer that causes inflammation in the breast. It tends to grow and spread quickly and may not cause a visible breast lump.
Symptoms of Breast Cancer
Symptoms of breast cancer may include:- A lump or thickening in the breast or underarm
- Changes in the size or shape of the breast
- Changes in the appearance of the breast, such as redness or dimpling
- Nipple discharge or a change in the appearance of the nipple
Diagnosis of Breast Cancer
The diagnostic process for breast cancer may include a physical exam, imaging tests, and a biopsy. A physical exam may include a breast exam and examination of the lymph nodes. Imaging tests, such as mammograms, ultrasound, and MRI, may be used to create detailed images of the breast and detect any abnormalities. A biopsy, in which a sample of tissue is removed and examined under a microscope, is often used to confirm the diagnosis of breast cancer.Stages of Breast Cancer
The stage of breast cancer refers to the size of the tumor and the extent to which it has spread in the body. The staging system for breast cancer includes:- Stage I: The cancer is small and has not spread beyond the breast.
- Stage II: The cancer is larger and may have spread to the lymph nodes near the breast. It may also be classified as either Stage IIA or Stage IIB based on the size of the tumor and the presence of cancer cells in the lymph nodes.
- Stage III: The cancer has spread to the lymph nodes in the armpit and may be present in the breast tissue as well. It may also be classified as either Stage IIIA, Stage IIIB, or Stage IIIC based on the extent of the cancer’s spread.
- Stage IV: The cancer has spread to other parts of the body, such as the liver, lungs, or bones.
Treatment Options for Breast Cancer
Treatment options for breast cancer may include:- Surgery: surgery is often the first line of treatment for breast cancer. This may include a lumpectomy, in which only the tumor and a small margin of surrounding tissue are removed, or a mastectomy, in which the entire breast is removed.
- Chemotherapy: chemotherapy uses drugs to kill cancer cells. It may be used before or after surgery, and may also be used in conjunction with other treatments.
- Radiation therapy: radiation therapy uses high-energy beams to kill cancer cells. It may be used after surgery to kill any remaining cancer cells, or as a standalone treatment for advanced breast cancer.
- Hormonal therapy: hormonal therapy is a type of treatment that targets hormones such as estrogen, which can fuel the growth of breast cancer cells. It may be used in postmenopausal women with estrogen receptor-positive breast cancer.
- Targeted therapy: targeted therapy is a type of treatment that targets specific genes or proteins in cancer cells. It may be used in combination with chemotherapy or as a standalone treatment.
- Immunotherapy: immunotherapy is a type of treatment that uses the body’s immune system to fight cancer cells. It may be used in combination with other treatments or as a standalone treatment.
Coping with Breast Cancer
Living with breast cancer can be a physical and emotional challenge. Treatment for breast cancer, such as surgery and chemotherapy, can cause side effects that can impact daily life. These may include fatigue, nausea, and changes in physical appearance. It is important to take care of oneself and seek support from loved ones, healthcare providers, and support groups to manage these challenges. Managing the impact of breast cancer on daily life, such as maintaining relationships and returning to work, may also be a concern. It is important to communicate with loved ones and employers about the impact of treatment and to make accommodations as needed. Seeking support from loved ones and healthcare providers can also be helpful in navigating the challenges of living with breast cancer.Conclusion
Breast cancer is a common type of cancer that can occur in both men and women . Early detection and personalized treatment are important for improving the chances of successful treatment and survival. There are several types of breast cancer, and the best course of treatment will depend on the individual situation. Living with breast cancer can be a physical and emotional challenge, and it is important to take care of oneself and seek support from loved ones and healthcare providers to manage these challenges.A scientist visits the doctor suspecting he has monkeypox. What happened next may surprise you…
The scientist thought he had monkeypox so he went to his primary care doctor. He says “I have rectal pain and swollen glands and want a monkeypox test.” The doctor says, “this looks and sounds a lot like an STD. I’m going to test you for a sexually transmitted disease instead.” But those tests came back negative and the pain was getting worse, so the scientist went to urgent care and asked again for the monkeypox test. As you might imagine, most urgent care don’t have this test available. Monkeypox is not like strep throat. It’s a disease that virtually no doctor in the USA has ever seen before. It’s only endemic in Africa. So the doctors at urgent care give him antibiotics to treat him instead for a bacterial infection. Well Monkeypox is viral. It doesn’t get better. It gets really bad. So bad that he can’t sleep at night. The scientist doesn’t give up, he goes to an ER at a big academic hospital in New York. He’s seen by specialists, but they don’t think it’s monkeypox either. They say they won’t test him for it. (It’s probably true that they didn’t test because they don’t have a way to test him for it and at this stage, they might have felt it wouldn’t change the treatment for his condition.) He must have been upset when a few days later, he got a rash, and its characteristic for monkeypox. When NPR published this story on May 25th, the number of cases in the entire USA was around 200 . Less than a month later, New York City alone has over 800 cases and that number is climbing.What is monkeypox?
Monkeypox is a zoonotic virus that affects animals and humans. It’s thought that the people of Sub-Saharan Africa have been affected by Monkeypox for thousands of years. Monkeypox was first isolated in a lab from infected monkeys in the late 1950’s in Africa. In the Democratic Republic of Congo in 1970 the first humans were infected by the same virus that was identified in 1950.Have there been prior outbreaks of monkeypox?
The first Monkeypox outbreak in the western hemisphere took place in the midwestern United States in 2003. According to the CDC, all of the 47 reported cases took place after direct contact with infected animals that were imported to the USA from Ghana.How does it spread?
Prior to the current outbreak most infections took place after contact with infected animals and the chance of spreading between people was low. But recent evidence suggests the current strain spreads between individuals especially in the MSM population.Are we dealing with a new more infectious strain of Monkeypox?
It’s a little concerning that the current infections are spreading more quickly and between people, that it has infected more individuals than in prior outbreaks and that it’s spreading across the globe. It’s possible that we are dealing with a new strain or that the virus has found its way into environments that make it easier to spread.Why are we underestimating case counts?
It seems many of the cases may be falling under the radar. We don’t know how many cases there are because we don’t have a good system of contact tracing for Monkeypox yet. It took a long time to set up this system to conduct contact tracing in COVID. Contact tracing is important to help notify people who were exposed get tested and treated more quickly.Staying Safe
To stay safe from monkeypox you can practice some of the same procedures you learned during the coronavirus pandemic. Practicing social distancing or wearing a mask if you are in an area with high prevalence or if you are living near someone who is infected is a good start. We have also learned that this is a disease that is spreading through close physical contact between individuals. It is also being spread during intercourse, according to the New York State Department of Health, so wearing protection during intimate activities is advised.How dangerous is Monkeypox?
Unfortunately, there is a wide range of reported mortality at this stage. There tends to be a bias towards higher mortality rates at the beginning of any outbreak. This was the case during the coronavirus pandemic which had extremely high mortality rates early on during the pandemic. While experts don’t think Monkeypox will spread like Coronavirus, no one really knows. Individuals, with multiple comorbidities, weakened immune systems as well as the elderly, young children and pregnant women are at greater risk from infection.Is Monekypox very contagious?
We don’t know. Monkeypox is not believed to have as high an R0 as Coronavirus, but it’s early. Initial testing done from CDC reported 30% positivity rates, suggesting it might be more contagious than we know. But those numbers may have been inflated by a limitation on tests or the populations that were tested. In other words, we need more data.The Silver Lining
The good news is that not only is there a test, there is also a vaccine. Monkeypox and smallpox are both part of the variola viral genus. This means that receiving a smallpox vaccine confers protection against Monkeypox.A few weeks ago, I woke up in the middle of the night, couldn’t sleep. It didn’t help that when I looked at my phone, I noticed a news story about a new variant of COVID thought to be more contagious than previous strains. The story about the B.1.1.529 strain or “Omicron” was morbid. It described that Omicron was tearing through South Africa, in a mostly unvaccinated population. Since COVID-19 hospitalizations and death tend to trail infections, it was too early to tell how bad things would be, but all indications were that it would not be good.What a difference a few weeks can make!
Predictions about how infectious, contagious or how fast Omicron spreads were accurate. However, what was surprising is that hospitalizations were not increasing at the same rate as the Delta variant or prior versions of COVID-19. Despite only 25% of the South African population having a vaccine intended to prevent severe illness, those who are infected are not experiencing high levels of severe disease or hospitalizations. Preliminary data of the first 43 documented cases of Omicron in South Africa showing there was only 1 hospitalization was promising. Recently published data shows there is a 70% – 80% reduction in the rate of hospitalizations with Omicron compared to earlier strains such as delta.
It’s not all good news. Omicron will infect more people, faster. Ultimately, this may increase overall hospitalizations despite a reduced rate of hospitalization, if it infects enough individuals. As is pointed out by Christina Ramirez, a biostatistician at the University of California, Los Angeles in an article in the NY Times, “I don’t want to be alarmist, but I don’t think that you can let your guard down.” Could another mutation exist that makes the virus more dangerous? I guess it is possible, though I doubt this is probable ( based on the statistical concept of reversion to mean – after all, most coronavirus or Coronaviridae are not deadly). If future versions of covid remain similar in nature to O-micron, there is a possible silver lining here, and it’s huge.
O-micron might achieve what the vaccine could not achieve on its own. Omicron can distribute itself effectively, not just in the USA, where there is an abundance of vaccinations and boosters, but globally where vaccines are scarce. In combination with a vaccine bringing COVID-19 antibodies to individuals without a prior exposure to COVID, O-micron infection will confer immunity to others. That could bring forward herd immunity, which takes place when enough individuals have antibodies. Given the lack of global distribution of vaccines, this was unlikely to take place any time soon, if not ever, from Vaccination and boosters alone. The O-micron variant might be the best thing we’ve seen in a long time! Only time will tell.
Vaccination rates in South Africa are around 25%

Initial CDC reports on Omicron suggested it might be less dangerous despite being more contageous

News outlets make sure they tamper any good news — here there is an emphasis on hospitalizations.

Herd immunity as defined by Mayo Clinic

The South African Study Shows lower rates of severe disease

The success in developing Coronavirus vaccines at “warp speed” can be matched by rapid administration. Disrupting the traditional model of vaccination can help facilitate a more rapid phased roll-out. Increasing the efficiency of vaccine administration usually aims to increase one-of-four distinct elements: the vaccine supply, number of venues, number of vaccinators or number of recipients. However, one simple solution, self-vaccination, can efficiently increase the venues, vaccinators and recipients simultaneously. It relies on trust and empowering the public to participate in the success of a vaccination campaign. Dr. Israel Weinstein, the orchestrator of one of the most successful mass vaccination campaigns in history, understood the value of relying on the public.

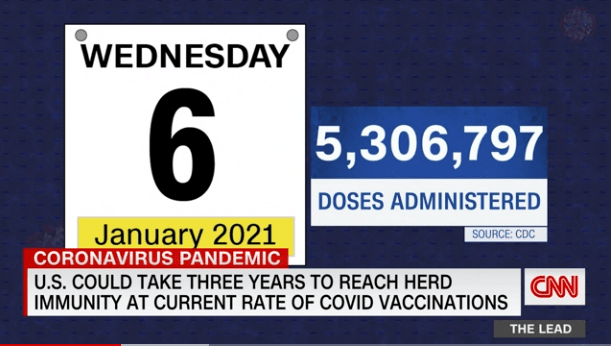
In 1947, under Dr. Weinstein’s leadership as health commissioner, New York City recruited volunteers and vaccinated over 5 million individuals for Smallpox in a period of 2 weeks. This was nearly 25 times the pace of the current vaccination effort, that vaccinated 300,000 New Yorkers in over 3 weeks. How was he able to achieve such success? Dr. Weinstein credited the “intelligent cooperation of the public” and “generous volunteers.” Over 73 years ago, he understood the public was intelligent, capable and needed to be central in a successful mass vaccination campaign. As of January 6th 2020, despite growing demand for a Coronavirus vaccine, nearly two-thirds of the vaccines delivered in the United States have not been administered. At this rate, it could take years to vaccinate the American public. To ensure the success of our current plan, we should learn from New York’s success in 1947, and rely on the public to play an increasing role.
Under the planned phased-vaccination roll-out of the US Government, the limited supply of vaccine is prioritized to at-risk populations. Tracking of vaccine allocation, ordering, uptake and management is web-based. As the volume of availability increases, vaccines will also become available at additional venues, some that may be efficient at vaccination like retail pharmacies that already give millions of flu shots every year. Should the planned venue expansion fail to relieve the current vaccination-rate bottleneck, mass outdoor vaccination sites such as stadiums may be used. Increasing the number of vaccinators by enlisting allied health professionals, might also speed administration. However, bureaucratic and regulatory hurdles are inherent in allowing these additional practitioners to administer a needle stick. Self-administration presents an alternative option, may overcome hurdles and can act synergistically with existing vaccination plans.
Research has shown self-vaccination from a prefilled syringe is safe, effective and that providing this option to individuals increases their intent to get a vaccine. Self-vaccination can take place independent of a traditional venue, freeing healthcare professionals to vaccinate others or care for sick patients. Alternatively, self-vaccination may incorporate the venue or participation of healthcare workers, if desired. In a designated healthcare location or a patient’s home via telemedicine participation, healthcare workers can provide further support, education, observation or documentation of self-vaccination. Similarly, vaccine tracking can be performed by self-vaccinators, participating healthcare providers or volunteers using existing IT web-based tracking systems using a computer or mobile phone.

Work is already underway to mass produce prefilled vaccine syringes, which among other advantages can save time, money and increase vaccine supply by up to 30%. Apiject, funded through Operation Warp Speed in May for this purpose, reports current capacity to prefill 45 million syringes per month and is working towards 250 million monthly capacity. Another company, currently preparing multidose-vials with Coronavirus vaccine, also has the ability to prepare prefilled syringes. Once fully FDA approved, large scale shipping of vaccines directly to individuals would be feasible. In the interim, manually prefilled syringes can be prepared from multi-dose vials. However, due to anticipated waste, these vials are intentionally overfilled, which is avoided when prefilling vaccine syringes. Self-administration of the injectable medication is not only a possibility, but a proven concept. Millions of Americans already have relevant experience with injectable medications and can contribute to a self-vaccination effort. Not only can these individuals—like the 10 million diabetics who inject insulin daily—self-vaccinate, they can assist others such as household members, relatives or friends. Additional participants in the self-vaccination effort can include medical professionals, pharmacists, phlebotomists, dentists, paramedics, veterinarians, and others with professional experience administering injections. By providing informal support to household members or others in their social network, they may bypass the licensure, professional or regulatory constraints that exist while working in their professional capacity. Many of these individuals might also be interested in contributing towards a more organized nationwide volunteer vaccination effort.

